Acquire the necessary skills outlined in the blog post for a nurse practitioner...
Read More
Discover the Critical Care Nurse Practitioner Course eligibility and skills, and...
Read More
Explore the process for becoming a Certified Registered Nurse Anesthetist (CRNA)...
Read More
Explore how Clinical Nurse Specialists positively impact healthcare delivery thr...
Read More
Discover the steps to become a Psychiatric Nurse Practitioner, including educati...
Read More
Discover the ways in which nurse practitioners make a difference in women's heal...
Read More
Stay ahead of the crowd by keeping these 5 points in mind when selecting your nu...
Read More
Unlock the potential of women's healthcare nurse practitioners with online life...
Read More
Discover why nurses in emergency medicine require life-saving courses to optimiz...
Read More
Learn the personality traits of a nurse and the benefits of online certification...
Read More
Learn the Requirement of Certification And Training for Nurse Practitioners. Tak...
Read More
A Critical Care Nurse Practitioner (CCNP) comes with specialized training and ex...
Read More
A psychiatric nurse practitioner plays an indispensable role in addressing the m...
Read More
This blog will tell you everything you need to know about Certified Registered N...
Read More
Explore psychiatric nurse practitioner certification and discover the degree opt...
Read More
In this article, we talk about the similarities and differences between CCNPs an...
Read More
Learn top tips to choose a nurse practitioner speciality and make a strong impac...
Read More
Know the top tips for aspiring nurse practitioners and students.
Read More
Learn the scope of practice for nurse practitioners.
Read More
Learn vital skills to learn in a nurse practitioner course
Read More
Learn how online life support certification for nurse practitioners is crucial i...
Read More
Continuing education is vital for registered nurses to stay current with medical...
Read More
From clinical expertise to effective communication, mastering essential skills l...
Read More
Explore the key differences between nurse practitioners and registered nurses, f...
Read More
To become a Registered Nurse (RN), follow these steps: earn a nursing degree, pa...
Read More
Continuing education keeps nurse practitioners up-to-date with medical advanceme...
Read More
Explore practical strategies for nurse practitioners to balance continuing educa...
Read More
Understanding mandatory vs. elective continuing education for nurses is essentia...
Read More
Curious about the impact of missing required continuing education for nurses? Le...
Read More
Discover the key differences between Physician Assistants and Nurse Practitioner...
Read More
Explore the key differences between Nurse Practitioners and Doctors, including t...
Read More
Becoming a nurse practitioner typically takes 6-8 years, including a bachelor's...
Read More
Can nurse practitioners prescribe medication? Discover the scope of their prescr...
Read More
Explore the key differences between Nurse Practitioners and Registered Nurses, f...
Read More
Discover the earning potential of registered nurses in the USA. Learn about aver...
Read More
Want to become a Pediatric RN? Earn a nursing degree, pass the NCLEX-RN, gain ex...
Read More.webp)
Wondering how to address a nurse practitioner? Learn the proper titles, professi...
Read More.webp)
Curious about nurse salaries in 2025? From RNs to NPs, explore pay trends, facto...
Read More
PCAs assist with daily living tasks like bathing and meal prep, while CNAs have...
Read More
Discover the steps to become an aesthetic nurse—from earning your RN license to...
Read More
Discover the steps to become a travel nurse, from education and licensing to lan...
Read More
ChatGPT said:Boost your nursing career with wound care certification. This guide...
Read More
Discover the top 5 online wound care certification programs of 2025—flexible, ac...
Read More
Confused between WOCN and wound certification? Discover the key differences in s...
Read More
Explore the top 6 continuing education options for wound care nurses to boost yo...
Read More
Prepare effectively for your wound care certification exam with these top study...
Read More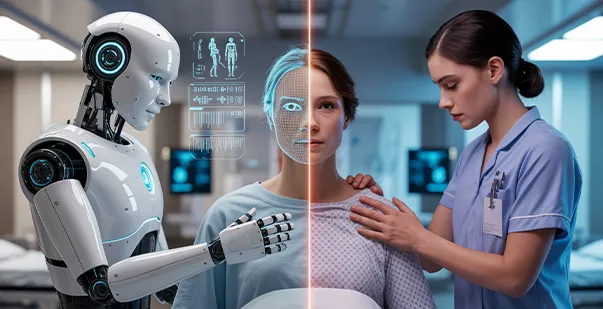
Explore how AI nurses are transforming healthcare — their benefits, risks, and t...
Read More
Wondering how many CEUs registered nurses need each year? Learn annual CEU requi...
Read More.webp)
Stay license-ready with ease. Learn simple ways to track your nursing CEUs, avoi...
Read More
Stay compliant and stress-free with our step-by-step guide to renewing your RN l...
Read More